Clinical Function of the SAIPH® Knee
- Products
- SAIPH® Knee System
- Clinical Function
Normal Pattern of Movement (Knee Kinematics)
Balancing stability with freedom of movement is a principal goal of TKR design. How well a TKR achieves this can be determined by evaluating the pattern of movement in patients’ knees during well-selected activities.
To evaluate the kinematics of the SAIPH® Knee, a consecutive series of one surgeon’s first 14 patients (mean 69 years old, range 51-83), with no exclusions were assessed using video fluoroscopy at a minimum 24 months postoperatively7. Study participants were asked to perform clinically relevant functional activities, including: a full internal-to-external pivot standing on the affected leg to show the AP extents of medial and lateral condyles with large torque while under load; a kneeling activity to establish full passive flexion; lunge and step-up/down activities to establish ROM and AP stability in both condyles for the loaded knee.
In all activities the SAIPH® Knee exhibited an asymmetric pattern of movement: the knee was AP stable on the medial side and lateral translation was permitted when required (Figure 1) 7.
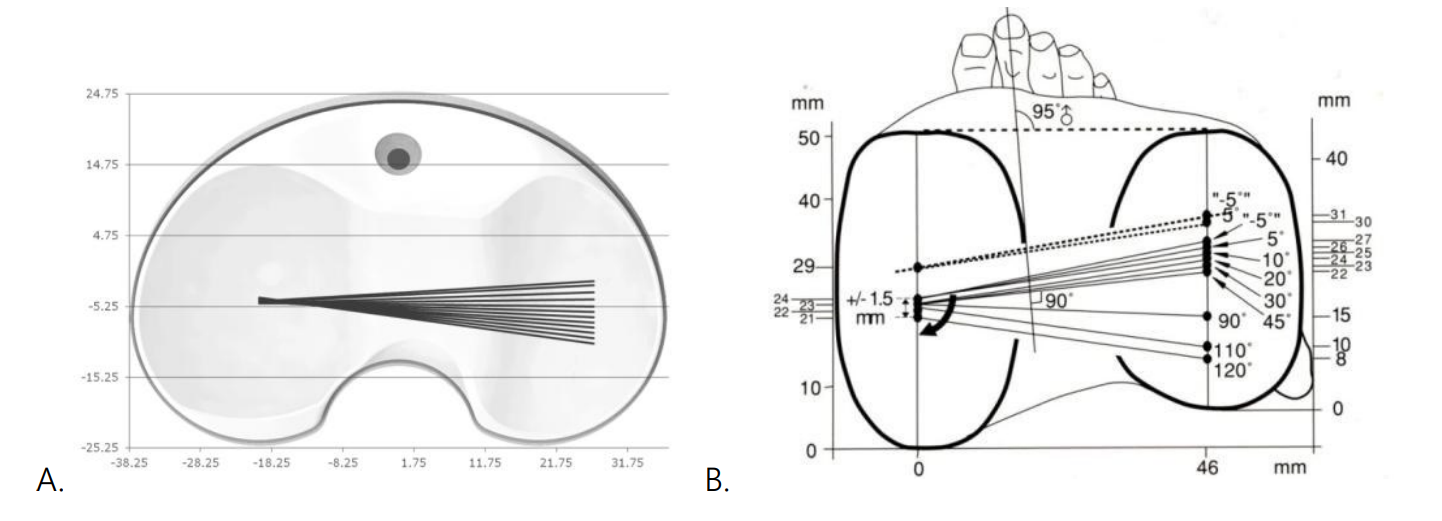
Figure 1 A. Near-normal freedom of movement in SAIPH® Knees: medial stability with lateral AP translation when required (data presented in Shimmin et al. 20157); B. A normal freedom of movement (Iwaki et al. 20003, Fig. 6a. ©2000 British Editorial Society of Bone and Joint Surgery. Reproduced with permission of the Licensor through PLSclear).
Stability
A ‘medial pivot’ design implies that a TKR should always exhibit a medial centre of rotation. But this is not the case: the normal knee centre of rotation is not static and, in some activities, lateral AP translation is suppressed4. The fundamental and essential characteristic of a normal knee is that it is always stable – throughout flexion. In the native knee, the provision of stability by the articular shapes and constraining tissues is greatest on the medial side but all compartments including the lateral and patellofemoral compartments contribute to stability.
If any compartment is neglected, the outcome is compromised. As such, the defining principle of MatOrtho® ball-and-socket knees is the provision of full-ROM stability. Because this is achieved with a medial deep-dish ball-and-socket articulation the concept is better termed ‘medially stabilised’. However overall stability is achieved with appropriate constraint in all compartments, and this is demonstrated by assessment of total knee AP stability throughout ROM.
Patients studied using fluoroscopic evaluation exhibited no paradoxical anterior translation of the femoral condyles during flexion in any activity, confirming the design intent for inherent full ROM stability (Figure 1) 7.
This feature is also confirmed in the 5-year follow up of 100 knees by Katchky et al., who found no incidence of symptomatic AP instability in patients30. In a study of 64 patients (mean age 72 years; mean follow-up 33.7 months) with four different knee designs (rotating platform LCS design, DePuy; cruciate retaining Triathlon, Stryker; medially stabilised knees SAIPH® Knee and MRK™, MatOrtho®) sagittal stability was measured at four degrees of flexion: 0°; 30°; 60°; and 90°, to examine the effect of design on mid-flexion stability33. Sagittal stability was similar in all four groups in full extension; however the MRK™ and SAIPH® Knee designs showed significantly improved stability in the midrange of flexion (30–60°) (Figure 2) 33.
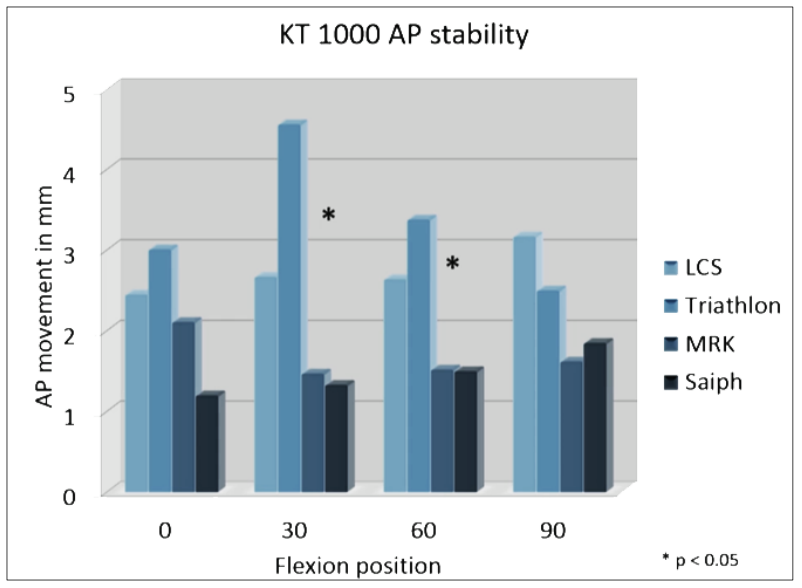
Figure 2 Sagittal stability for 4 knee designs at different degrees of flexion33.
In a separate similar study of 60 patients with four TKR designs (medially stabilised, cruciate retaining ‘1’, cruciate retaining ‘2’ and cruciate retaining ‘deep dish’) sagittal stability was measured using the KT1000 at 30° and 90°27.
Patients were recruited from three centres (three surgeons each implanting 10 SAIPH® Knees and 10 comparative knees). Patients were matched for age, gender, BMI and time to follow-up. When comparing medially stabilised knees (SAIPH® Knee) to cruciate retaining ‘1’ knees, AP movement was significantly less in the SAIPH® Knees at both 30° (p=0.037) and 90° (p=0.030)27. When comparing SAIPH® Knees to cruciate retaining ‘2’ knees, AP movement was significantly less in the SAIPH® Knees at 30° (p=0.013) and less at 90° although not significant (p=0.156)27. When comparing SAIPH® Knees to cruciate retaining ‘deep dish’ knees, AP movement was significantly less in the SAIPH® Knees at both 30° (p=0.030) and 90° (p=0.048)27. When comparing all SAIPH® Knees to all non-medially stabilised knees, AP movement was significantly less in the SAIPH® Knees at both 30° (p=0.003) and 90° (p=0.008)27.
To compare surgeons’ perception of sagittal anteroposterior (AP) stability after total knee replacement, 60 videos were taken of an AP drawer test of 60 patients performed by an examiner who was blinded as to what knee design each patient had received. Nine surgeons, who were blinded as to what knee design each video presented, were asked to grade the stability of all knees by determining whether they exhibited <5mm, 5-10mm or >10mm AP translation. Results demonstrated that the SAIPH® Knees were consistently perceived to be more stable than the cruciate retaining and ‘deep dish’ designs: 74% stable SAIPH® Knees vs. 38-40% other knee types (Figure 3) 27.
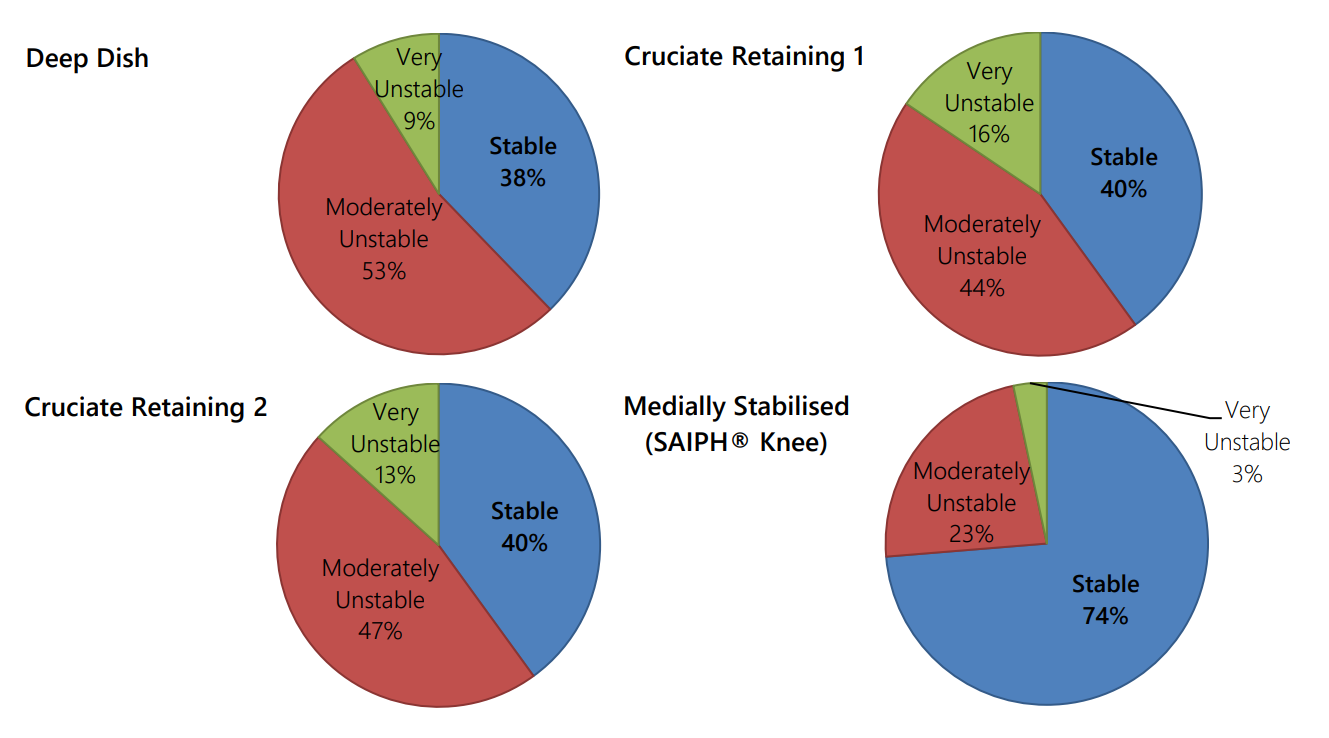
Figure 3 Stability assessment of 60 patients with four designs of knee, finding 74% of SAIPH® Knees were stable in contrast
to 40% or less for other knee designs27.
References
4. Hill PF, Vedi V, Williams A, Iwaki H, Pinskerova V, Freeman MA. Tibiofemoral movement 2: the loaded and unloaded living knee studied by MRI. J Bone Joint Surg Br. 2000; 82(8):1196-8.
7. Shimmin A, Martinez Martos S, Owens J, Iorgulescu AD, Banks S. Fluoroscopic motion study confirming the stability of a medial pivot design total knee arthroplasty. The Knee. 2015; 22(6): 522-526.
27. Jacobs H, Jones C, Brighton R, Redgment A, Talbot S and Walter WL. Sagittal Stability: KT1000 and PROMs. Presented at the Forever Active Forum, Valencia, 2019.
29. Walter WL, Shimmin A, Richards L and McDonald L. SAIPH® Medial Ball and Socket Knee: 2-year Follow-Up of the First 200 Patients. Presented at the AOA ASM, Brisbane, 2016.
30. Katchky AM, Jones CW, Walter WL, Shimmin AS. Medial ball and socket total knee arthroplasty. Five-year clinical results. Bone Joint J. 2019; 101-B (1 Supple A): 59-65.
33. Munir S, Molloy D, Hasted T, Jack CM, Shimmin A and Walter WL. Sagittal Stability in Four Different Knee Designs. A Single Centre Independent Review. Orthopaedic Proceedings. 2016; 98-B (SUPP 4): 113. Presented at ISTA 27th Annual Congress, Kyoto, 2014.
Resources
SAIPH® Clinical Rationale
SAIPH® Flyer
SAIPH® Operative Technique
Download Now
Fill in your details below to download the SAIPH® Clinical Rationale
Additional Text
Download Now
Fill in your details below to download the SAIPH® Flyer.
Additional Text
Download Now
Fill in your details below to download the SAIPH® Operative Technique
Additional Text
Patient Reported Outcome Measures (PROMs)
In their 2-year follow up study, Walter et al. used a visual analogue scale (VAS) for patient satisfaction and found that 95.3% responded positively (responding 8-10 on a 10-point scale), which they commented was unusual in their previous knee cohorts and was equivalent to satisfaction responses for their own hip cohorts (95.2%) at the same timepoint29.