Benefits of Hip Resurfacing
- Products
- ADEPT® Hip Resurfacing System
- Benefits of Hip Resurfacing
The benefits of hip resurfacing include:
- A viable treatment for younger, more active patients
- Early intervention
- Bone conserving procedure
- More reliably restored native hip joint biomechanics4
- Lower infection rates5
- Lower incidence of dislocation4
- Improvements in activity levels and hip scores, particularly in younger patients4,6
- Ease of femoral revision
Return to sport and leisure activities
Resurfacing of the femoral head allows for better restoration of the anatomy4,7 and may be more natural under stressed gait conditions such as high walking speeds, push-off forces and hill walking when compared to conventional THR8,9. Expert surgeons allow their hip resurfacing patients to return to a wider variety of sport and leisure activities without restriction as compared to total hip replacement, and return to activity is commonly much earlier in the postoperative recovery phase4, 10,11. Patients report a high level of activity including running4,6, 8 ,13,13 and these levels of activity may be maintained into the second decade after primary surgery13,14,15,16.
Reduces the risk of dislocation
Hip resurfacing allows the safe use of large-diameter head components, which offers an immediate advantage for the patient in terms of stability, and significantly reduces the risk of dislocation that is associated with THR4. In the UK National Joint Registry (NJR) the incidence rate of revision for dislocation within the first postoperative year is estimated at 2.5 to 4.5 times less for hip resurfacing than for THR and remains low at later time points5.
More conservative than THR
Hip resurfacing is a more conservative procedure than THR, with no requirement to ream deep into the femoral shaft, which may reduce exposure to bacteria. The UK NJR shows that a hip resurfacing procedure is 1.3 to 1.9 times less likely to be revised within one year for infection than a THR5 . The benefits of reducing the risk of infection are far-reaching: revision for infection is associated with twice the costs and length of stay in hospital as compared to revision for aseptic causes17, and is associated with a higher level of complication, reoperation and morbidity17. Hip resurfacing also has a lower risk of mortality when compared to THR18,19.
Revision of hip resurfacing
Revision following a conventional THR is invariably more challenging, more expensive and takes longer than the primary procedure, despite the many specialist techniques to address the problems at revision surgery. Retention of the femoral neck and an uncompromised femoral shaft means that revising a hip resurfacing is essentially conversion to a primary total hip replacement, with similar technology, expense and potentially the same postoperative recovery to a conventional primary THR. This is more appealing to younger patients who are more likely to require a repeat surgery in their lifetime.
Lower risk of mortality
Resurfacing devices are used more commonly in younger, more active patients and there are numerous confounding risks for mortality rates; nevertheless, there is a growing body of evidence supporting the observation that mortality rates are lower for hip resurfacing when compared to THR. The Australian Joint Registry reported in 201920 that hip resurfacing patients have 1.5 times and 1.8 times higher rates of survival beyond 15 and 18 years respectively compared to THR patients after adjusting for age and gender (Figure 3). Published studies also describe lower mortality rates in the long term when a hip resurfacing implant is used, especially in male patients under 55 years of age at surgery21,22,23.
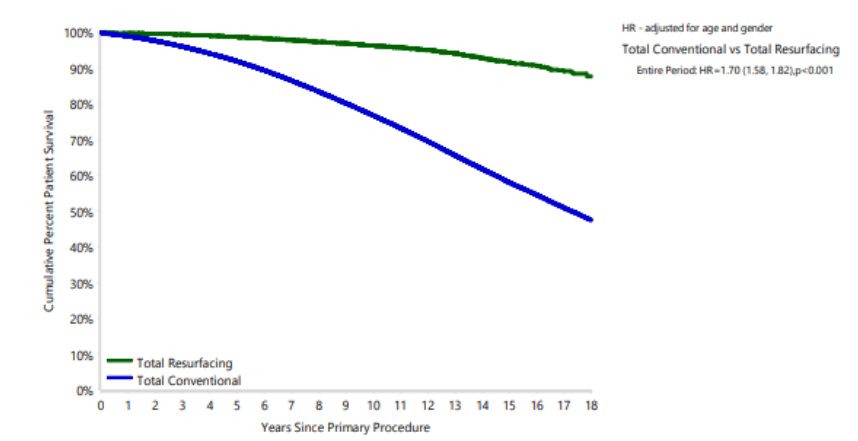
Figure 3: Cumulative percent survival of patients receiving hip resurfacing or THR20
References
3. McMinn D. The History of Hip Resurfacing.
4. Hellman MD, Ford MC, Barrack RL. Is there evidence to support an indication for surface replacement arthroplasty? A systematic review. Bone Joint J. 2019; 101-B (1 supple A): 32-40.
5. National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. 18th Annual Report, 2021: Surgical data to 31 December 2020. www.njrreports.org.uk.
6. Barrack RL, Ruh EL, Berend ME, Della Valle CJ, Engh A Jr, Parvizi J, Clohisy JC, Nunley RM. Do Young, Active Patients Perceive Advantages After Surface Replacement Compared to Cementless Total Hip Arthroplasty? Clin Orthop Relat Res. 2013; 471: 3803–3813
7. Lombardi AV Jr, Skeels MD, Berend KR, Adams JB, Franchi OJ. Do large heads enhance stability and restore native anatomy in primary total hip arthroplasty? Clin Orthop Relat Res. 2011; 469(6): 1547-53.
8. Maillot C, Auvinet E, Harman C, Cobb J, Rivière C. Hip resurfacing generates a more physiological gait than total hip replacement: A case-control study. Orthop Traumatol Surg Res. 2020. 106(3):527-534.
9. Aqil A, Drabu R, Bergmann JH, Masjedi M, Manning V, Andrews B, Muirhead-Allwood SK, Cobb JP. The gait of patients with one resurfacing and one replacement hip: a single blinded controlled study. Int Orthop. 2013; 37 (5): 795-801.
10. Van Der Straeten C, De Smet KA. Current expert views on metal-on-metal hip resurfacing arthroplasty. Consensus of the 6th advanced Hip resurfacing course, Ghent, Belgium, May 2014. Hip Int. 2016; 26 (1):1-7.
11. Girard J. Femoral head diameter considerations for primary total hip arthroplasty. Orthop Traumatol Surg Res. 2015; 101 (1 Suppl): S25-9.
12. Plate JF, Issa K, Wright C, Szczech BW, Kapadia BH, Banerjee S, Mont MA. Patient activity after total hip arthroplasty: a comparison of three different bearing surfaces. J Long Term Eff Med Implants. 2013; 23(4): 315-21.
13. Haddad FS, Konan S, Tahmassebi J. A prospective comparative study of cementless total hip arthroplasty and hip resurfacing in patients under the age of 55 years A Ten-Year Follow-Up. Bone Joint J. 2015; 97-B: 617–22.
14. Girard J, Miletic B, Deny A, Migaud H, Fouilleron N. Can patients return to high-impact physical activities after hip resurfacing? A prospective study. International orthopaedics. 2013; 37(6):1019-24. 15 Rueckl K, Liebich A, Bechler U, Springer B, Rudert M, Boettner F. Return to sports after hip resurfacing versus total hip arthroplasty: a mid-term case control study. Archives of orthopaedic and trauma surgery. 2020 Jul; 140(7):957-62.
16. Common H, Rousseau R, Putman S, Migaud H, Girard J. High-level judo practice after hip resurfacing. Orthopaedics & Traumatology: Surgery & Research. 2020; 106(8):1511-4. 17 Vanhegan IS, Malik AK, Jayakumar P, Ul Islam S, Haddad FS. A financial analysis of revision hip arthroplasty: the economic burden in relation to the national tariff. J Bone Joint Surg Br. 2012; 94 (5):619-23.
18. Kendal AR, Prieto-Alhambra D, Arden NK, Carr A, Judge A. Mortality rates at 10 years after metal-on-metal hip resurfacing compared with total hip replacement in England: retrospective cohort analysis of hospital episode statistics. BMJ. 2013; 347: f6549.
19. Australian Orthopaedic Association National Joint Replacement Registry. Hip, Knee & Shoulder Arthroplasty: 2021 Annual Report. Adelaide: AOA. 2021. https://aoanjrr.sahmri.com.
20. Australian Orthopaedic Association National Joint Replacement Registry. Supplementary Report, Mortality of Hip and Knee Arthroplasty. Adelaide: AOA. 2019.
21. Kendal AR, Prieto-Alhambra D, Arden NK, Carr A, Judge A. Mortality rates at 10 years after metal-on-metal hip resurfacing compared with total hip replacement in England: retrospective cohort analysis of hospital episode statistics. BMJ. 2013. 27; 347.
22. McMinn DJ, Snell KI, Daniel J, Treacy RB, Pynsent PB, Riley RD. Mortality and implant revision rates of hip arthroplasty in patients with osteoarthritis: registry based cohort study. BMJ. 2012. 14; 344.
23. Jonas SC, Whitehouse MR, Bick S, Bannister GC, Baker RP. An 18-year comparison of hybrid total hip replacement and Birmingham Hip Resurfacing in active young patients. HIP International. 2019; 29(6):630-7.
Resources
ADEPT® Clinical Rationale
ADEPT® Flyer
ADEPT® Operative Technique
Download Now
Fill in your details below to download the ADEPT® Clinical Rationale
Additional Text
Download Now
Fill in your details below to download the ADEPT® Flyer.
Additional Text
Download Now
Fill in your details below to download the ADEPT® Operative Technique